Improving personalised prevention at Hack Healthcare
The coming Hack Healthcare event is focused on improving healthcare by tackling challenges in four themes:
- Personalized prevention
- Beyond telemedicine
- Data value chains
- Alternative financing models
Roche has taken the lead on the personalised prevention theme, focusing on three specific challenges:
- Better health choices everyday, to empower individuals diagnosed with early-stage neurodegenerative diseases to manage their conditions over the long term by providing them with data-driven insights and recommendations.
- Trigger health check-ups, to increase frequency of healthy citizens of doing regular check-ups by leveraging behavioural science in collaboration with health insurers, employers and the more traditional healthcare actors.
- Unleash predictive analytics, to trigger consultations with general practitioners (GPs) or specialists, or a contact with a tele-consultation provider based on anomalies detected in behavioural, exercise or nutrition data from a wide range of data sources.
We thought that the best way to introduce this personalised prevention track of the Hack Healthcare hackathon would be to start by interviewing Celia Oculi, Personalised Healthcare Lead at Roche Belgium, whose background is in biotechnology, pharmacy and marketing.
Why does prevention need to change, and why now?
Prevention has always existed. We know that we have to eat 5 fruits and vegetables per day, our mums told us that and our grandmothers said it earlier to our mums. It is the one size fit all vision of healthcare! What has changed is that all stakeholders are now aligned on the fact that prevention is key. This is enabled by personalised healthcare to ensure a treatment addresses the right segment of patient that will respond best to a given treatment and tailor the care path. Expertise in different disciplines converge to accelerate progress in personalised healthcare. Some of these trends, for example advances in our understanding of the biology of disease, and the growing availability of real world data and electronic health records, are game changers. The current pandemic has also accelerated innovation, and showed how crucial it is to invest in healthcare to prepare for the future. We know that if we work towards a healthcare system that treats earlier, enables preventative care and avoids unnecessary therapies, we will then ensure financial resources are optimally spent where they have the greatest impact for the benefit of the patients.
What is personalised prevention exactly and how is it different from “regular” prevention?
Personalised prevention is the opposite to the “one size fits all” model of “you need to eat 5 fruits and vegetables per day. It refers to efforts to prevent disease at the level of the individual. It complements classic population-based public health efforts, but is based on biological measurements (genomic and biomarkers). You look at individual medical evidence to tailor the most optimal care. If you take the example of cancer, it is no longer seen as just one disease, but a collection of hundreds of diseases, each with unique characteristics and its own genetic make-up. With what we call “tumor agnostic” therapies we are now looking at the disease at the molecular level to understand the best way to treat it, regardless of where it first originated. We recently celebrated World Cancer Day, and know that 40% of cancers could be prevented while it is the most deadly disease. Our ambition for lung cancer for instance is to contribute to eradicate it by 2040: on one side by preventing the 95% of cases that are preventable (due to smoking or environmental factors) and on the other hand by diagnosing the other 5% as early as possible to provide them with the best care possible.
What underlying problems does personalised prevention solve?
Personalised prevention enables clinicians and the industry to understand the roots of the disease with the specificity of each patient as well as having the possibility to intervene at the earliest stage with curating technologies. It is a game changer, enabling the shift from sick care to healthcare, and from curative to preventive care. What is needed to do that is evidence with medical data. The scale of the problem therefore lies in the belief that sharing medical data is a bad thing. We are willing to divulge all kinds of private information to an airline in exchange for travel to our destination but we hesitate to give private information to the healthcare industry, who could provide us with far more life-changing services from this information. Our genomic makeup is what truly differentiates us as individuals: we hold the keys to unlock the genomic information inside all of us, and in providing it to the industry that will develop effective medicines and treatments that help us as individuals. Of course, genomic information is the most personal of all personal data. Consequently, the healthcare industry must treat this information with the utmost respect and ethics. It must enter into a clear and honest dialogue with people to explain how data is to be used and the benefits it will ‘pay back’ in return for this highly privileged access.
What is enabling this trend?
The emergence of molecular information, made possible by advances in the field of DNA sequencing and the ability to collect and process larger amounts of data quickly, together with the increasing number of wearable technologies and measurement devices, integrated “around” your body and habits and in your house. These technologies capture and monitor several parameters of our health constantly.
If the promise of the impact of personalised prevention is so relevant, why hasn’t it happened yet? What are the challenges that you see in making these bottlenecks go away?
There is currently no infrastructure to enable the intake of personalised healthcare in Belgium, and there is a need for alignment among all healthcare stakeholders on this issue. The healthcare system in Belgium is fragmented between communal, regional and federal, not to mention the differences between North and South. The pandemic shed the spotlight on 8 ministers responsible for health in our little country! We need to break those silos to have a system approach where everyone that has an impact on prevention is involved (healthcare professionals, payers, policy, industry) and put in place incentives to nudge this. Access to data is an area where Belgium could improve as we only rank 21st out of 34 countries if you look at the personalised healthcare index of the Future Proofing healthcare initiative. We hope such a tool will enable Belgian policymakers and key stakeholders to better understand the strengths of our health system (of which there are many) and where we can improve. 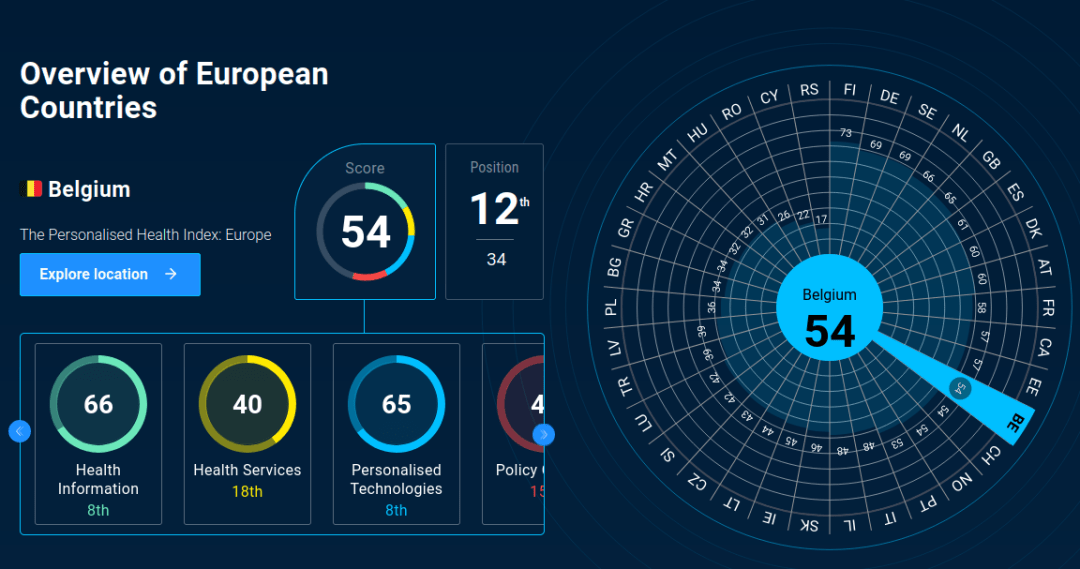 Roche calls for the establishment of trustworthy data infrastructures and methods to enable large scale collection, storage and sharing of health data. We advocate for instance for the integration and increased interoperability of hospital data warehouses. Belgium has taken the first steps in creating such a culture by its ambition of establishing a National Health Data Authority and we support this very much. A strong data culture focused on capability and innovation are necessary to be successful in recommending value-based treatments. More work finally needs to be done in promoting trust among citizens as regards sharing or anonymised health data to enable better patient outcomes, increased R&D in novel medicines and healthcare systems efficiencies.
Roche calls for the establishment of trustworthy data infrastructures and methods to enable large scale collection, storage and sharing of health data. We advocate for instance for the integration and increased interoperability of hospital data warehouses. Belgium has taken the first steps in creating such a culture by its ambition of establishing a National Health Data Authority and we support this very much. A strong data culture focused on capability and innovation are necessary to be successful in recommending value-based treatments. More work finally needs to be done in promoting trust among citizens as regards sharing or anonymised health data to enable better patient outcomes, increased R&D in novel medicines and healthcare systems efficiencies.
Who are the potential partners with whom you could work to make it happen?
Roche believes that collaboration is tomorrow’s modus operandi in healthcare. We need to better connect existing healthcare players and combine technologies in innovative ways – both to sustain innovation and ensure ongoing delivery of healthcare. The pandemic has shown the need and the ability to innovate in record time, at scale, and has unleashed an unprecedented level of global collaboration and partnership – companies, regulators and governments most work together closely to improve care and drive innovation. One great example we have in Belgium is our partnership with Sciensano and the Belgian Society of Medical Oncology. It demonstrates the impact of the personalised healthcare approach for oncology patients via the GeNeo initiative. It is an unprecedented collaboration because different organizations that sit together to address the different perspectives of personalised medicine (technologies, incentives, reimbursement, follow up care, etc). We are all concerned by prevention, so we are happy to collaborate with everyone that is active in prevention and who wants to volunteer. That’s why we run this hackathon open to all. And most importantly, we need the decision-makers to make it happen.
Why is Roche so focused on personalised prevention?
Personalised healthcare is a strategic priority at Roche as we aim to give the right treatment to the right patient at the right time. Timing is critical here as we can predict the onset of Alzheimer’s symptoms 10 to 15 years upfront (Jack C. et al. (2013) Lancet Neurol; 12(2):207-216) Today we don’t have solid therapeutic solutions to offer to patients but in the future new treatments will arrive and should be available to patients before any progression of the disease. Roche’s business model is to be 100% committed to innovation, and specifically to looking for new molecules to help patients with major unmet medical needs. Roche is a healthcare company that specialises in both diagnostic and pharmaceutical innovation. The coordination between the two parts of our Roche Group makes us truly unique as it ensures that we can provide patients with optimal assistance throughout their entire journey: diagnosis, prevention, detection, monitoring, support in treatment choices, medicines, etc.
About Roche
Roche is a global pioneer in pharmaceuticals and diagnostics focused on advancing science to improve people’s lives. The combined strengths of pharmaceuticals and diagnostics under one roof have made Roche the leader in personalised healthcare – a strategy that aims to fit the right treatment to each patient in the best way possible. Roche is the world’s largest biotech company, with truly differentiated medicines in oncology, immunology, infectious diseases, ophthalmology and diseases of the central nervous system. Roche is also the world leader in in vitro diagnostics and tissue-based cancer diagnostics, and a frontrunner in diabetes management. Founded in 1896, Roche continues to search for better ways to prevent, diagnose and treat diseases and make a sustainable contribution to society. The company also aims to improve patient access to medical innovations by working with all relevant stakeholders. Thirty medicines developed by Roche are included in the World Health Organization Model Lists of Essential Medicines, among them life-saving antibiotics, antimalarials and cancer medicines. Roche has been recognised as the Group Leader in sustainability within the Pharmaceuticals, Biotechnology & Life Sciences Industry ten years in a row by the Dow Jones Sustainability Indices (DJSI). Learn more about Roche Belgium.
Are you or your organisation interested in improving personalised prevention? Get your Hack Healthcare ticket and get ready for two days that will rock the world.



Recent Comments